UnitedHealthcare (UHC) is one of the largest health insurance providers in the United States, offering coverage to millions of members across all 50 states.
Healthcare providers must initiate the payor enrollment process early to serve United Healthcare-insured patients and receive reimbursements. However, processing times for provider enrollment vary by state due to regulatory requirements, application volume, and administrative processes. Starting the process early puts you in control and ensures a smoother experience.
This guide provides a detailed, state-by-state breakdown of United Healthcare enrollment processing times. As you read, you’ll discover the reasons behind these variations and strategies for optimizing the process.
Understanding UHC Regional Processing
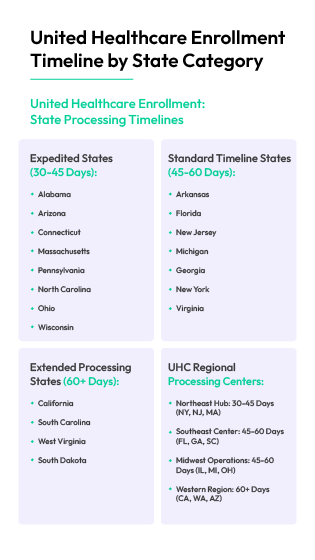
United Healthcare operates through several regional hubs, each with its processing timelines and requirements.
These regions include:
1. Northeast Hub
The Northeast region includes New York, New Jersey, and Massachusetts. Processing times in this area are generally quicker, averaging 30–45 days, due to efficient electronic systems and centralized operations that minimize delays.
2. Southeast Center
The Southeast region covers states such as Florida, Georgia, and South Carolina and experiences moderate processing times, typically ranging from 45 to 60 days. However, high provider volumes in states like Florida can occasionally lead to backlogs.
3. Midwest Operations
The Midwest hub encompasses states like Illinois, Michigan, and Ohio. Processing times vary based on state-specific Medicaid requirements, but most applications are processed in 45–60 days.
4. Western Region
The Western region includes states such as California, Washington, and Arizona. Due to complex licensing and payer-specific documentation requirements, processing times in this area often exceed 60 days.
UnitedHealthcare State Processing Categories
United Healthcare enrollment processing times can be divided into three categories: expedited states, which typically take 30-45 days; standard timeline states, which usually take 45-60 days; and extended processing states, which often exceed 60 days. Understanding which category your state falls into can help you better prepare for the enrollment process.
1. Expedited States (30–45 Days)
List of States
These states have efficient enrollment processing due to well-established credentialing systems.
Requirements for Fast Processing
- Submitting complete and accurate applications
- Using electronic applications and online portals over paper submissions
- Ensuring up-to-date credentialing through CAQH ProView
- Following up within 10–15 days after submission
- Ensuring work history, hospital privileges, and peer references are validated
Success Factors
- Avoid simple mistakes like incorrect NPI numbers or missing signatures
- Double-check all information before submission
- Use a credentialing specialist to manage the process and prevent delays
Common Pitfalls
- Lack of malpractice insurance documentation
- Not utilizing electronic submission options
- Omitting updated copies of state licenses, DEA registration, or malpractice coverage
- Neglecting to use CAQH ProView for automated provider data entry
- Failing to check in with UHC within 10–15 days post-submission
- Inconsistencies in work history, NPI numbers, or practice address details
2. Standard Timeline States (45–60 Days)
List of States
Documentation Needs
- State medical license(s)
- DEA registration
- Board certifications
- Professional liability insurance
- Work history (5 years) and hospital privileges
- Current state medical license(s) and attestation
Optimization Tips
- Submit applications at least 90 days before the provider’s start date
- Confirm document requirements with United Healthcare’s provider portal
- Follow up regularly to track application progress
3. Extended Processing States (60+ Days)
List of States
Additional Requirements
- Complete employment history with explanations for any gaps between 6 months and above
- Additional verification for certain specialties
- Proof of active hospital privileges
Risk Mitigation
- Start the enrollment process at least 120 days in advance
- Double-check all submitted documents for completeness
- Contact a United Healthcare supervisor if delays exceed expected timelines
Critical Success Factors for UHC Enrollment
Successfully enrolling with United Healthcare health plan requires a proactive approach to documentation and follow-ups.

Below are some critical factors to keep in mind
1. Documentation Requirements
Proper documentation is the foundation of a successful UHC enrollment application.
Ensuring all required forms and supporting documents are submitted correctly is a responsibility that prevents unnecessary delays. It's a testament to your diligence and commitment to the process.
Essential Forms
- Provider Portal Login: This is the first step to take. The portal registration includes creating a healthcare ID, signing in, connecting your TIN, and navigating the portal
- CAQH ProView Attestation: This form verifies provider information and records updates in the centralized credentialing database. Attestation must be completed within 14 days of submitting the enrollment application
- State-Specific Medicaid Enrollment Forms: If required, providers applying for Medicaid programs may need to submit extra documentation
Supporting Documents
- Active state medical license(s)
- Board certifications
- DEA registration
- Malpractice insurance certificates
- Work history verification
Validation Requirements
- Primary Source Validation: All credentials should be confirmed directly with the original issuing authority, such as licensing boards or medical organizations
- Data Accuracy Review: Verify that names, dates, and identification numbers are consistent across all documents to avoid processing issues
- Notarization (if applicable): Certain states mandate notarized copies of specific forms for verification purposes
Submission Formats
- Electronic submission (preferred method via CAQH ProView or United Healthcare portals)
- Faxed submissions (only if accepted by the state plan)
- Paper-based applications (least preferred, but required in some cases)
2. Follow-Up Protocols
Regular follow-ups help prevent unnecessary delays and ensure applications stay on track. Below are protocols to follow:
Optimal Timing
- First follow-up: 15 days after submission
- Regular status checks: Every two weeks until final approval
- Escalation: If there is no response within 60 days, escalate to a United Healthcare supervisor
Contact Strategies
- Preferred Contact Methods: Start with an email, then follow up with a phone call
- Direct Provider Relations Team: Alternatively, you can contact UHC’s provider enrollment department to avoid delays
Resolution Tracking
- Keep a Follow-Up Record: Document all interactions, noting dates, contact details, and response updates
- Monitor Outstanding Applications: Identify and prioritize cases that need immediate attention or remain unresolved
- Update Processing Timelines: Revise tracking systems to align with the latest estimated completion times based on received feedback
Processing Optimization Tips
Providers should focus on meticulous preparation, diligent tracking, and effective troubleshooting to minimize delays and expedite approvals.
The following strategies can help streamline the enrollment process.
1. Pre-Submission Preparation
Ensuring a strong foundation begins with compiling accurate and complete applications before submission.
Essential Documents
- Fully completed United Healthcare provider enrollment application
- Copy of valid state licenses and board certifications
- DEA registration (if required)
- Malpractice insurance certificate with up-to-date coverage
- Work history with explanations for any gaps
- Hospital privileges documentation (if applicable)
- Specialty-specific credentials, such as Medicare/Medicaid enrollment forms
Verification Process
- Confirm educational background and training
- Validate state licensure
- Verify board certifications
- Cross-check work history and malpractice records
- Ensure hospital privileges and references are accurate
Avoiding Common Errors
- Complete all application fields to prevent processing delays
- Submit documents in the required format (e.g., PDF instead of Word)
- Check expiration dates to ensure all licenses and certifications are current
- Avoid discrepancies in provider names or practice addresses
Quality Assurance Measures
- Conduct an internal review before submitting applications
- Ensure all required documentation is included by using a checklist.
- Have a second reviewer verify provider details for accuracy
2. Managing the Timeline
Real-time tracking of applications helps prevent unnecessary hold-ups. Below are best practices for managing processing times efficiently.
Tracking Methods
- Use credentialing dashboards to monitor application status
- Maintain a shared document with submission dates, follow-ups, and expected timelines
- Check United Healthcare provider portals for live updates on application progress
Confirming Status
- Follow up with United Healthcare 15 days after submission to verify receipt
- Continue follow-ups every two weeks until processing is complete
- Request written confirmation once the application is approved
Expediting the Process
- Submit applications during less busy periods to avoid seasonal backlogs (e.g., avoid December, January, and July)
- For urgent cases, submit a formal expedited request with supporting documentation
- Ensure all required documents are included from the start to avoid unnecessary resubmissions
- Use automation tools to track key deadlines and receive alerts for pending items
Practical Resources
Wrapping Up on Blue Cross Blue Shield Payor Enrollment
Successfully enrolling with United Healthcare requires a proactive approach to documentation, tracking, and follow-ups. Healthcare organizations that adhere to structured processes and meet all requirements upfront experience fewer delays and rejections.
Consider using credentialing platforms that simplify licensing, payor enrollment, and provider network management for a more seamless enrollment experience.
Book a FREE demo with a credentialing specialist to get started today.



.png)

.png)


